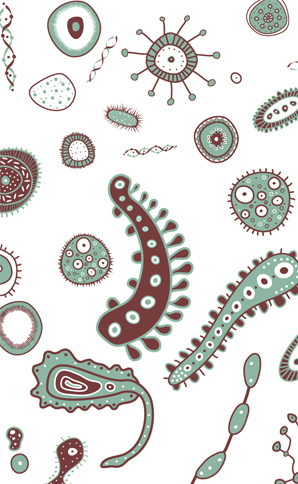
We are vastly, ridiculously, hopelessly, humblingly outnumbered: For every one human cell, there are an estimated 10 single-cell microbes in us or on us, at least 100 trillion in all, nestled in our guts and in our urogenital tracts, lying on our skin and happily ensconced in our mouths and noses—entire civilizations of fungi and protozoa and (mostly) bacteria that eat and breathe, evolve and reproduce and die.
Before you reach in horror for the hand sanitizer or industrial-strength mouthwash, you might want to keep something in mind. A profusion of research in just the past five years is showing that our microbial hitchhikers, collectively called the “human microbiota” and so small they account for only 1 or 2 percent of our weight, play a key role in maintaining our health. And we disrupt them at our peril. “It’s not possible to understand human health and disease without exploring the massive community of microorganisms we carry around with us,” says Professor George Weinstock of Washington University in St. Louis. Knowing which microbes live in healthy people “allows us to better investigate what goes awry in diseases that are thought to have a microbial link, like Crohn’s and obesity.”
The microbes in our body—especially some of the 10,000 or so species of bacteria in and on us—have indeed been implicated in disorders as diverse as obesity and Crohn’s, and also in asthma, heart disease, sinusitis, and possibly even mood disorders. They influence how big our appetite is and, possibly, even what foods we crave. They synthesize vitamins and affect how quickly we metabolize drugs such as acetaminophen (Tylenol), they protect against esophageal reflux and they churn out many of the same neurochemicals as our own brains. Given this job description, it’s hardly surprising that when perturbed, scientists are discovering, the microbiota can tip us into poor health or outright illness.
Exactly how our bacterial companions affect our health is the subject of ongoing research in labs around the world, but one thing is clear: Our decades-long war on germs is looking seriously wrongheaded. In an effort to obliterate disease-causing microbes through antibiotics and anti-microbials—from the pills we down for a cold (against which antibiotics are useless) to the meat we eat to the hand-sanitizer-dispensers everywhere you look—we are carpet-bombing our microbiota. And that war on germs takes a huge toll on beneficial bugs, too.
One example: The bacterium Helicobacter pylori causes ulcers and has been linked to stomach cancers. Although it was once in almost everyone’s gut, it is now found in just 6 percent of U.S. children, Science magazine reported in 2011, probably due to the widespread use of antibiotics and anti-microbials. That should mean fewer ulcers, but there’s a dark lining to that silver cloud: H. pylori may ward off asthma. Scientists led by Dr. Martin Blaser of New York University Langone Medical Center found that those without H. pylori are more likely to have had childhood asthma than those with it. Coincidence? In 2011 scientists in Switzerland infected half of a colony of mice with the bacteria and left the other half germ-free. They showered all the mice with dust mites and other allergens. Mice with H. pylori were fine; those without suffered airway inflammation, the hallmark of asthma.
Exactly how H. pylori might ward off asthma is still a mystery, but researchers have made progress understanding the link between our microbiota and other diseases.
The field of microbiota and health took off in 2006, when scientists led by Jeffrey Gordon of Washington University in St. Louis noticed something: Fat mice and svelte mice have very different gut microbes. Could different microbes actually cause obesity? To find out, Gordon transferred gut bacteria called Firmicutes from obese mice into thin ones. The thin mice ate no more than they used to, but they quickly started packing on the pounds (okay, ounces). Firmicutes, it turns out, are really good at liberating calories from food, much better than the common gut bugs called Bacteroidetes. That finding offers a hint of why your friend can scarf down calories and remain slim while you have merely to walk past a bakery window to gain weight. “Some microbes change how efficiently we metabolize food,” says biologist Rob Knight of the University of Colorado, who studies the genetics of the microbiota, called the microbiome.
It seems Firmicutes are quite adept at digesting fats and carbs, allowing you to absorb many more of, say, the 1,200 calories in half of a Domino’s bacon-cheeseburger pizza than if you have fewer Firmicutes and more Bacteroidetes. “Obesity depends not just on calories ingested but also on the microbiome,” says Dr. Yang-Xin Fu of the University of Chicago Medicine. And, yes, like mice, obese people tend to have more Firmicutes and fewer Bacteroidetes than slim people.
At this point everyone asks, how can I get my slim friend’s menagerie of gut microbes? Short answer: Scientists don’t know yet. But they have some clues. For instance, Bacteroidetes—the microbes linked to slimness—proliferate in the presence of fructans, a form of fructose found in asparagus, artichokes, garlic, and onions, among other foods, notes microbiologist Andrew Gewirtz of Georgia State University. A diet high in fructans might support a good crop of slimming Bacteroidetes. On the other hand, he notes, stress decreases the abundance of Bacteroidetes, suggesting one more way stress causes obesity.
“Lots of people are exploring the possibility of using antibiotics or prebiotics or probiotics to treat obesity,” says Colorado’s Knight. Prebiotics are foods that promote the growth of some bacteria at the expense of others. Probiotics are live microorganisms such as the Lactobacillus in yogurt; the idea is to ingest beneficial ones. The strategy with antibiotics would be similar: Zap the obesity-promoting ones. These ideas are in their very earliest stages, so don’t go looking on your drugstore shelves for such products just yet.
Much clearer is the strong evidence that modern medicine’s penchant for antibiotics has a downside beyond the well-known problem of breeding antibiotic-resistant bugs. A study of 11,532 children found that, on average, those exposed to antibiotics for the usual childhood ills, such as ear infections, from birth to 5 months of age weighed more for their height than other kids. By 38 months, they had a 22 percent greater likelihood of being overweight, scientists reported last August. “The rise of obesity around the world is coincident with widespread antibiotic use,” says Blaser. “It is possible that early exposure to antibiotics primes children for obesity later in life.” That’s one reason farmers add antibiotics to animal feed: The drugs alter the gut bacteria in cattle, pigs, and others, substituting bacteria that are better at extracting maximum calories from feed and thereby making the animals pack on the pounds.
Become a Saturday Evening Post member and enjoy unlimited access. Subscribe now