We breathe about 12 to 20 times a minute, without having to think. Inhale, and air flows through the mouth and nose, into the trachea. The bronchi stem out like a wishbone, and keep branching, dividing and dividing, and finally feeding out into the tiny air sacs of alveoli. Capillaries — blood vessels thinner than hairs — twine around each alveolus. Both the air sac and the blood vessel are tiny, delicate, one cell thick: portals where blood (the atmosphere of the body) meets air (atmosphere of the world). Oxygen passes from air to blood; carbon dioxide, from blood to air. Then, the exhale pushes that carbon dioxide back out the mouth and nose. Capillaries channel newly oxygenated blood back to the heart. That oxygen fuels the body. That’s why we breathe.
Today, these basics of human respiration and metabolism feel obvious — and ventilators, the machines that breathe for sick people, do too. We have so many medical devices, so of course we’d need, and have, machines that help us to breathe. But there’s a strange, and deeply human, story behind how we learned to breathe for each other. It starts long ago, when we didn’t understand breathing at all. When the body’s failure to breathe was incomprehensible, incurable, and fatal. When we had no way of knowing how badly we needed ventilators to keep people alive through those moments of vulnerability, lest those moments be their last.
Medical TV shows have accustomed us to the sight of doctors moving quickly to keep the sickest patients alive — but that link between hurry and success hasn’t always existed. Up to 100-odd years ago, for most of human history, when doctors had a dying patient, they rushed to do what they knew, but the patient died anyway. It doesn’t matter if you hurry or move slowly if your “cures” don’t work. Ventilation, the linchpin of critical care medicine, changed that. Doctors could save some of the dying. That new technology helped bring medicine from hopes and crossed fingers to saving lives.
It is surprising, though, how long it took us to understand breathing. Through much of the 19th century, doctors believed that a lack of stimulation made patients lose consciousness. Methods of attempted resuscitation included rolling patients over barrels, hanging them upside down, cooling them on ice, throwing them onto a trotting horse, flagellation, or using the fumigator, in which smoke was blown up the patient’s rectum. The list sounds more like hazing for fraternity pledges than medical care.
When did we start getting it right? As usual with scientific progress, there’s no one moment of absolute clarity, and moments of partial lucidity were misinterpreted or forgotten over the years. Take Galen, a physician to gladiators in the Roman Empire during the second century. Galen’s key discovery was the physiology — the very mechanism — of breathing. We think of lungs as the body part that breathes. The lungs receive the breath, yes, but they don’t breathe, the verb, the action. Breathing takes muscle — specifically the diaphragm, the thin dome of muscle nested at the base of the lungs.
Relaxed, the diaphragm forms two shallow upside-down bowls, one beneath each lung. To cue an inhale, the diaphragm contracts. The upside-down bowls flatten into upside-down plates. The diaphragm takes up less space in the chest cavity, leaving a void, and air rushes into the nose and mouth, filling that space. That expands the lungs, equalizing the pressure in the chest. The diaphragm relaxes, the plates rise into bowls, and an exhale follows.
Galen described that system of anatomy accurately — but he also wrote an inaccurate explanation of the heart and the circulation of blood.
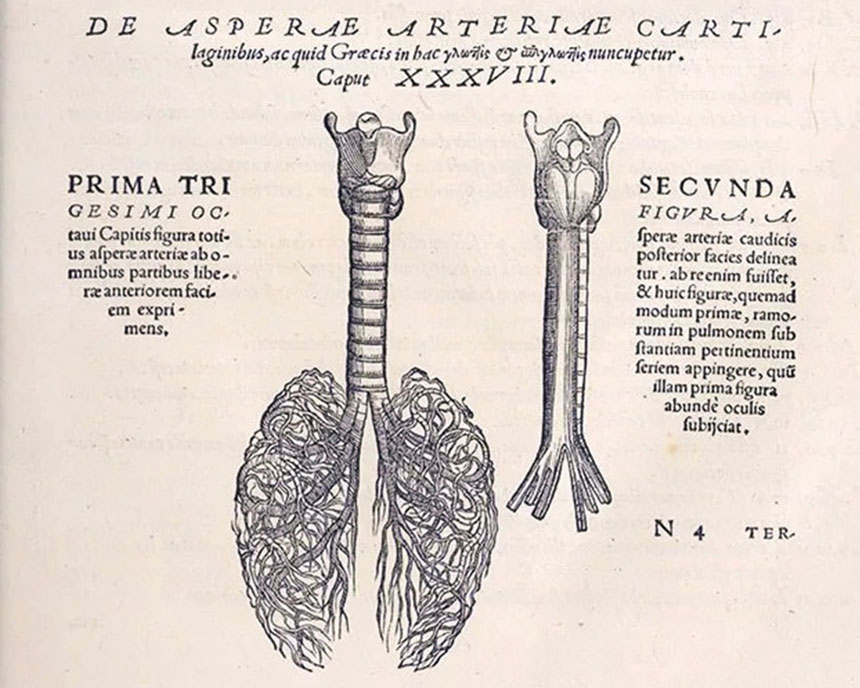
The 16th-century Flemish physician Andreas Vesalius corrected Galen’s misconceptions about blood circulation by repeating Galen’s live pig dissections as well as dissections of human corpses. Through such experiments Vesalius, often referenced as a Father of Anatomy, wrote about a pioneering experiment in the science of mechanical ventilation:
[A]n opening must be attempted in the trunk of the arteria aspera [trachea], into which a tube of reed or cane should be put; you will then blow into this, so that the lung may rise again and the animal take in the air … the lung will swell to the full extent of the thoracic cavity, and the heart become strong and exhibit a wondrous variety of motions.
Vesalius had performed the first documented experiment in ventilation, but he didn’t know it at the time. Scientists back then still didn’t understand that breathing brought fuel into the body, let alone what that fuel, oxygen, did.
Scientists grasped what oxygen is, and how the body uses it as fuel, in 1774. That knowledge gave doctors the last puzzle piece they needed to understand breathing — both its mechanism and its purpose — and to build machines that supported breathing when it failed.
In those days, breathing was life. We now have the concept of “brain death”: that someone can die of a lack of brain function while a ventilator keeps the body breathing, animated, approximating life. Back then, though, whatever the cause of death — injury, or sickness, or simply old age — a dead person was a person who no longer breathed. So doctors searched for ways to keep patients breathing. In the 1800s, they finally understood human physiology well enough to build machines that could work. They needed only to engineer them.
In 1838, the Scottish physician John Dalziel published an idea: He’d prototyped a machine that could push air in and out, much like the body itself. The patient squatted inside a sealed box, with only the head and neck sticking out. A device Dalziel called a piston — it looked like a bike tire pump — sucked air out of the box, making a vacuum. Air could get into the box only through the patient’s mouth and nose. This was the first mechanical negative pressure ventilator, forcing the patient to inhale, just as the diaphragm does in a healthy person’s body. When Dalziel tried his machine on a healthy person, air “rushed along the air-passages and distended the chest without effort.”
Soon, fellow clinicians and inventors were trying to -create designs that could keep the sick alive, but each attempt had flaws.
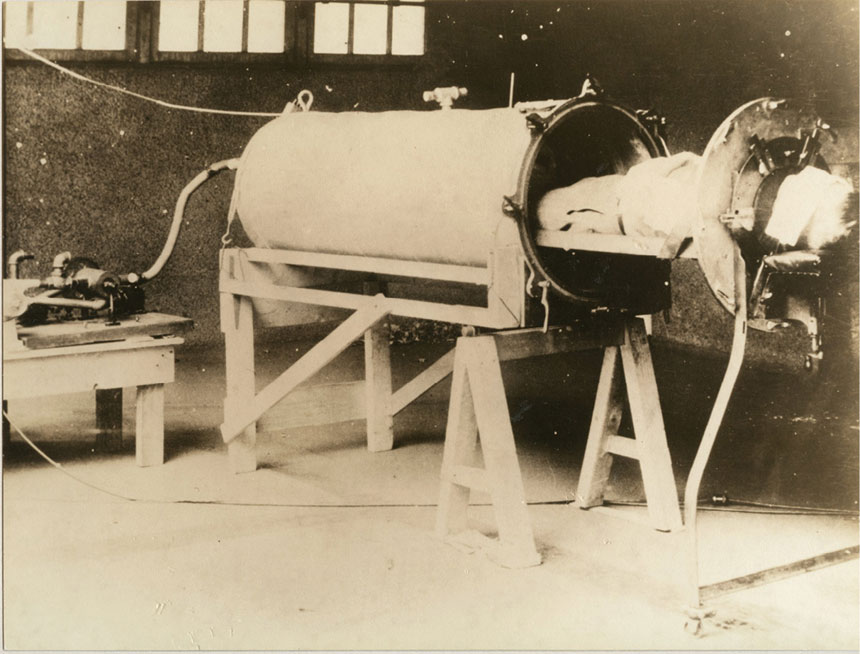
Finally, in 1929, a pair of Harvard doctors, Philip Drinker and Louis Agassiz Shaw, built a negative pressure mechanical ventilator that kept sick patients alive: the iron lung. The patient lies inside the machine, with only the head exposed. Early versions required an operator to hand-pump air in and out; the later versions — the ones that still keep patients alive today — are automated. The machines use the same principle as Dalziel’s. The nickname iron lung is actually somewhat of a misnomer because the machine replaces the functioning not of the lung but of the muscles that fill and empty it — but the iron diaphragm doesn’t have the same ring.
The machines worked — though far from perfectly. They were expensive, cumbersome, and fussy. And, while some hospitals had plenty of iron lungs, others didn’t. Doctors needed stockpiles of the machines, now called ventilators, in case of epidemics. They -— doctors, hospitals, cities, countries, governments — weren’t prepared for emergencies.
Between August and December 1952, around 3,000 patients in Copenhagen were rushed to hospital. They had a constellation of similar symptoms. Some were sicker than others. The sickest couldn’t breathe. There was no cure, and no prevention but the avoidance of the already sick. Doctors struggled to keep patients alive. Almost all of the sickest people died.
The story resounds to an earlier echo of Wuhan in 2019, but the disease in Copenhagen in 1952 was poliomyelitis (polio). Copenhagen had hosted an international conference of polio doctors in 1951. They’d come to learn from each other about the disease. There was so much they didn’t know. They didn’t know, for example, that many of them carried it.
The conference ended. The polio doctors left. The disease stayed and spread. The next year, sick patients came to the Blegdam Hospital: first some, then many, then too many.
In the first three weeks of what doctors later recognized as an epidemic, 31 patients with breathing and swallowing paralysis came to Blegdam; 27 of them died. It was the largest-ever polio epidemic in Europe to date. Henry Cai Alexander Lassen, the doctor in charge, called the situation a “state of war.” New patients came in sick, got sicker, died. The doctors grew desperate for any possible cure.
A senior resident, Mogens Bjørneboe, thought he knew someone who could help: the anesthesiologist Bjørn Ibsen, who arrived at Blegdam on a Monday morning. Lassen and Bjørneboe brought him to the autopsy room, where Ibsen examined a 12-year-old boy who had a high level of carbon dioxide in his blood. Ibsen had read about high levels of carbon dioxide in patients needing ventilation, and remembered a paper on polio patients in Los Angeles kept alive with the technique.
The Copenhagen hospital had a handful of negative pressure ventilators on hand. But the L.A. study described another sort of ventilation: positive pressure. It’s like inflating a balloon. Negative pressure ventilators (the human body, the iron lung) enclose the balloon in an airtight box and suck the air out of the box. Air flows into the mouth of the balloon. With positive pressure, you blow air directly into the balloon.
The practice is used to this day. Anesthesia medications administered so that patients go under also paralyze the diaphragm. Breathing goes out with consciousness, so doctors keep patients alive through positive pressure ventilation during surgery. They breathe for the patients while the patients can’t breathe for themselves.
Ibsen himself had done this during surgery. First, he performed a tracheotomy: a slice into the patient’s throat, with care not to nick the carotid artery. Then, he slid a tube through the cut, into the patient’s windpipe. The other end of the tube either connected to an oxygen tank or fed out into ambient air. Along the tube, between patient and air supply, was a squeezable rubber ball. Compressing the ball with a fist pushed air into the patient’s lungs. Release, and the air moved back out. That was “hand bagging,” a method of ventilation so rudimentary that it’s strange to call it a technology.
Ibsen asked for a chance to try the technique on the very sickest polio patients at Blegdam, those who would otherwise die. Despite grave reservations, Lassen picked Vivi, a 12-year-old girl who was almost gone. Vivi’s sickness had started with fever, a headache, and stiffness in her neck. The day she came to the hospital, doctors asked her to move her hands, maybe make a fist, or just wiggle her fingers. She couldn’t. Soon, she gasped with each breath. She had liquid, her own secretions, in her lungs. She wasn’t underwater, but she was drowning.
An ear, nose, and throat specialist at Blegdam sliced open Vivi’s throat and slid a tube into her windpipe. The records don’t say who did it, maybe because it didn’t go well; Ibsen later said, “a colleague lost a lot of time during the tracheotomy. When eventually it came to my turn, I got confronted with bronchospasm and panicking, making the intubation impossible.” As Vivi spasmed and bucked, Ibsen, the anesthesiologist, administered phenobarbital, a short-term sedative. Vivi collapsed. She stopped moving, stopped breathing.

Blegdam’s doctors left the room. Ibsen stood over Vivi’s body, the two of them alone. He had to save this patient. He said later that “a failure of a demonstration would probably confirm the epidemiologists’ belief that the situation was hopeless.” One chance to help Vivi — and then, the hundreds of patients like her.
Ibsen kept working. He suctioned mucus from Vivi’s lungs, then pumped the rubber ball, once, twice, three times, four. Each push forced air into her lungs. Her chest and belly lifted, sank, lifted, sank.
The Blegdam doctors walked back in — and got a shock. Vivi was “warm, dry, and pink.” Remembering the day decades later, Ibsen said, “That I could save the patient’s life with such a simple method was one of the most incredible moments of my life.”
Why did it work? The accumulated carbon dioxide had caused the patient’s organs to fail. Breathing requires not just oxygen entering the lungs with each inhale, but also carbon dioxide exiting with each exhale. Blegdam’s iron lung patients weren’t exhaling fully, so the carbon dioxide couldn’t escape. Doctors tried administering oxygen, but they really needed to find a way to facilitate the exhale of carbon dioxide. Ibsen’s positive pressure ventilation did that, where the iron lung couldn’t.
Blegdam now needed to ventilate an ever-rising number of polio patients with shortness of breath. Teams of clinicians would need to hand-bag them, day and night, until recovery. Blegdam had a solution, but also too many patients, and not enough hands.
In just a few days, the clinicians made and implemented a plan. Medical students became human ventilators, in the same way that NASA’s mathematicians were human calculators. Some 1,500 students worked six- to eight-hour shifts, with a 10-minute smoke-break every hour. Students kept the same patient assignments day after day, until their patient either breathed alone or died. Students and patients formed close bonds, because their patients stayed conscious. Modern ventilator machines can work through intubation: a tube passing through the patient’s mouth. It’s less invasive than a tracheotomy. But the body rebels at a tube in the throat, so doctors keep intubated patients unconscious. Blegdam’s patients were awake. The student sat by the patient all night, sharing air, life, in such proximity — yet the patient could slip into death. Many of the medical students burned out and quit.
Following the Copenhagen epidemic, another wave of clinicians and engineers designed new ventilators, with positive pressure this time.
Soon, motion begat motion. Blegdam gathered patients needing ventilation into one area, the first Intensive Care Unit (ICU). Ibsen started sending doctors to ride with medical transportation for critically ill patients, so that they could ventilate them during transport. In the midst of a terrifying epidemic, critical care medicine was born.
Inspiration is a tired word. We overuse it, on refrigerator magnets and those depressing motivational posters on office walls. We forget its origins: It means getting a new urge or idea, yes, but it also meant inhalation. To inhale: to breathe motion into stasis. To animate. Animation is not sufficient for life — in the history of ventilation, so many doctors have ventilated the dead — but it is necessary. All the inventions in the world remain useless until we learn how to use them. In the chaotic muddle, as people fell ill and died, doctors had long had the tools to keep some of those people alive. They needed to animate their systems.
That was the obstacle to care then, but what about now? Ventilators have been automated for decades — but, in anticipating the COVID-19 pandemic, American doctors and ethicists wondered if they should plan for ventilation by hand, if they ran out of machines.
Robert Truog, who directs the Harvard Medical School Center for Bioethics, co-wrote the Massachusetts guidelines on rationing ventilators in April 2020. He and his colleagues considered giving the families of patients removed from ventilators the option to hand-ventilate their sick family member, as students had done with Blegdam’s patients nearly 70 years before. The ethicists decided not to offer families that option, says Truog, citing three issues: burdening family members unrealistically; medical complications that would likely result from the efforts of untrained human “ventilators”; and, finally, the likelihood that those patients wouldn’t survive anyway.
The first two complications applied to Ibsen’s efforts at Blegdam, too: It was logistically difficult to muster a large enough group of volunteers to continuously ventilate so many patients, and Blegdam’s untrained human “ventilators” made mistakes.
The third complication did affect Ibsen’s work, but he didn’t know it, because there wasn’t a name for it yet. Truog is referring to the concept of medical futility: moments when doctors decide not to offer certain interventions because those interventions won’t help the patient enough to justify the harms. Futility is the most common ethical dilemma in the modern ICU. The question guiding care becomes not just how to save lives, but when to allow deaths. Not just animating machines, but deciding when to use them, and when not to.
Before physicians understood how people breathed, they couldn’t help people to continue breathing. They tried anyway — and all of their efforts, though well-intended, constituted futile care: interventions not reasonably likely to bring more good than harm. The term futility didn’t exist not because the problem didn’t yet exist, but because the problem was too big to see. Scientifically sound ventilation methods changed that.
Now, doctors can prolong life — but not always in a condition that patients would choose to live with. We have to ask: What quality of life would we consider worth living? If the best possible medical care can’t give a patient a reasonable quality of life, patients and their physicians decide to withdraw or discontinue further treatment. We see it on medical shows — characters say, Don’t keep me on a machine. They often mean a ventilator. The more advanced and effective the ventilator has become, the more questions of futility arise.
The more we learn about respiratory failure in patients, the more we realize that different types of respiratory failure require different types of ventilation. The machines deliver an amazing array of ways of giving a breath. Ventilators can also monitor patients’ ever-changing vitals and automatically adjust to their needs. But, the more sophisticated the ventilator, the more that could go wrong.
Future ventilators will be even more complex. A journal article on the past, present, and future of the ventilator declares: “The key term that will be used to identify future ventilators will be smart!” The machine will assess its own performance and might even help to decide whether its use is futile or not.
How much can, or should, the ventilators of the future help doctors make decisions about when to turn off machines? The ventilator, once a caring human using arm muscles as proxy for patients’ paralyzed diaphragms, is now a programmed device — and that programming could someday make decisions of life and death. The machines that have extended life might, in time, help to determine when it ends.
Sarah Ruth Bates is a writer, author, and teacher. Her work has appeared in the Boston Globe Magazine, The New York Times, Guernica, Aeon, and elsewhere. For more, visit sarahruthbates.com.
This article is featured in the September/October 2023 issue of The Saturday Evening Post. Subscribe to the magazine for more art, inspiring stories, fiction, humor, and features from our archives.
Become a Saturday Evening Post member and enjoy unlimited access. Subscribe now