Golf legend Jack Nicklaus readily admits the path to becoming one of the greatest golfers of the 20th century wasn’t without pain and sacrifice–particularly in the hip. It may come as a surprise to many that the “Golden Bear” achieved such a remarkable string of victories while suffering from intense debilitating hip-joint pain. In 1963, while playing the final hole of a pro tournament, Nicklaus missed an approach shot and suffered such pain in his left hip that he was forced to endure 23 cortisone injections over a 10-week period.
Initially, Nicklaus shrugged off his osteoarthritis pain, believing it a minor annoyance rather than something that would eventually define his life. But over time, the chronic pain chipped away at even routine and pleasurable activities.
Nicklaus–in company with such celebrities as Elizabeth Taylor, Charlton Heston, Mike Ditka, and Luciano Pavarotti–is one of the estimated 375,000 Americans who undergo hip replacement surgery each year, according to the American Academy of Orthopaedic Surgeons (AAOS). Experts project this number will continue to rise as the population ages.
To learn more about the procedure and advancements in technology and techniques that are making the procedure less invasive and recovery speedier, the Post spoke with Joseph C. McCarthy, who was recently elected to the Board of Directors of the AAOS and who is currently clinical professor of orthopedic surgery at Tufts University School of Medicine and staff orthopedic surgeon at New England Baptist Hospital, specializing in hip replacement surgery.
What are the most common reasons for hip replacement?
McCarthy: In general, the most important and common reason is incapacitating pain unrelieved by conventional rest or anti-inflammatory medicines. The second reason is restricted flexibility or motion of the hip joint, resulting in limitation in bending or flexing of the hip–motions used to sit, squat, climb stairs, or twist the knee, such as when bending down to put on your shoes or socks or getting in and out of a car. The third reason relates to specific activities that individuals are unable to do, such as when a young athlete is unable to run a marathon or an older person is unable to climb stairs or pick up a grandchild.
What conditions contribute to deterioration of the hip joint?
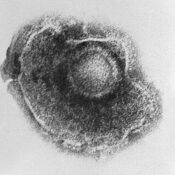
McCarthy: The most common cause of chronic hip pain and disability is arthritis. In osteoarthritis, for example, the cartilage cushion, or cap, on the top of the bone of the ball-and-socket joint is worn down like a bald tire, producing pain, restricted motion, and limited function. Trauma may also cause the same problem.
Many people today participate in sports, such as jogging or tennis, to promote a healthier lifestyle, but do some sports exact a greater toil on hip joints?
McCarthy: What is healthy for maintaining the flexibility and tone of the leg muscles may not necessarily be healthy for the joint. When your foot hits the ground, force is transmitted to the hip joint. When walking, the force is about three times your body weight. So when a 200-pound man walks, he puts about 600 pounds of force across his hip joint with each step. During running, the force is between five and six times one’s body weight per step–in a 200-pound person that equates to a half-ton per step, Forces transmitted to the joint are much higher than people would believe, and the cartilage in the hip joint employed to withstand that force is amazingly thin–only three or four millimeters thick on the ball and on the socket at adolescence.
Over time and with use, there is gradual thinning of the cartilage due to the tons of force that we place on our joints during day-to-day life–especially in activities such as jogging. People who jog in adolescence and early adulthood often report feeling a tremendous exhilaration. Given the accumulated force that the sport puts on hip joints, however, it is astonishing that the joints hold up as well as they do. As physicians, we often see joggers in their 50s or 60s, when the joint cartilage has worn down to the bone. While jogging is a wonderful activity, most physicians who see patients with arthritis would suggest that it is best not to focus on only one type of exercise. Cross training, Pilates, pool therapy, and yoga improve flexibility and include stretching activities. By working arms and shoulders one day, legs on another, and swimming the following–in other words varying the routine–you distribute the load, use different muscle groups, and don’t overwhelm the hip.
What advances in hip replacement technology have improved outcomes?
McCarthy: In the ’60s and early ’70s, hip replacement was done as a cemented prosthesis. The stem, which goes into the femur and the cup that the ball rubs on, basically needed to be fixed to the bone. At the time, there was only one way to do that–with bone cement or glue that to this day is still used, although less frequently.
In the 1980s, cementless implants that attach directly to bone without glue were developed, representing a remarkable advance. Most implants were form-fitted into the bone; however, further developments led to better attachment surfaces. Since the ’70s, the stem and the cup have been made of much stronger metals–chrome cobalt and titanium. Although refined over the years, these metals remain the two state-of-the-art materials used for the stem and the cup. They have proven to be strong, durable, resistant to breakage, and biocompatible.
The most recent advances involve what’s called the bearing surfaces-the ball that goes on top of the stem and the liner to replace the worn-out cartilage. In the ’60s and ’70s, the only bearing surface available was either cast chrome cobalt or titanium femoral heads. Over the years, the plastic liner has gone through improvements in manufacturing so that it’s much stronger, more resistant to wear, and more durable. Metal on metal couples–meaning the ball is made of a chrome cobalt and the socket liner is made of the exact same material polished and matched exactly in its geometry to the ball–wear at an extremely low rate. The ceramic-on-ceramic replacements are exact matches and incredibly hard and smooth materials. The wear rate for ceramics is slightly less than the metal on metal, but both are extremely low. There is a substantial increased cost to make metal-on-metal bearings and ceramic-on-ceramic bearings so they are most frequently used in younger, active people, where the replacements will theoretically last longer throughout the course of their lives.
In short, the implants used today are more commonly cement-less, or what’s called bony in-growth, than they were in years before, which hopefully will provide more lasting attachment to bone. And an increasing number of people are using one of the three fancy-bearing surfaces–the highly cross-linked polyethylene, the metal-metal, or the ceramic-ceramic.
What advancements in surgical technique have occurred?
McCarthy: There are many different surgical approaches to the hip joint–from the back, from the side, or from the front. In the ’70s, virtually every hip replacement required that the surgeon take off the muscle and bone from the trochanter (located on the femur). Leg muscles on the side really prevent you from getting to the hip. Surgeons used to remove a piece of bone along with the muscle to which it was attached so that they could access the hip joint to do the procedure. Later, people developed ways to sneak behind the muscles called the gluteus medius and minimus–together known as the abductor muscles that are on your side and important for walking. Surgeons developed methods of preserving the muscles by going behind them and not taking off the bone through a standard posterior approach, which would entail a fairly long incision. Another method emerged where you enter in front of the hip, called an anterior approach to the hip, again through a pretty long incision. The ability to preserve the abductor muscles is not only understood, but also more universally practiced.
Over the last five years, hip incisions for a standard total hip replacement have become shorter. The length of the incision has been reduced from on average 20-25 centimeters (8-plus inches) to about 8 to 12 centimeters (4 or less inches) in length. The muscle is still preserved, whether you go through the back or the front, just as it was with the longer incision. The joint capsule, which is literally the lining of the hip joint that used to be removed to perform the operation, is not taken out. We preserve and repair it. The prosthetic joint is more stable, which reduces the risk of dislocation.
Today, the healing time is also shorter. We are able to get a patient up earlier after surgery because we don’t have to wait for the capsule to heal. These advances have helped improve the recovery of the hip, allowing patients to get up sooner and walk with more confidence and less fear.
Given the emergence of new technology and techniques, is it advisable to seek a center of excellence where many hip replacement procedures are performed?
McCarthy: People who live in a rural community may go to a local hospital simply because it’s convenient for family to visit. However, a person would be best served by, at the very least, getting a second opinion at a center of excellence or a high-volume joint replacement center by a physician with experience in the procedure and whose judgment they trust.
Do pre-existing health conditions like diabetes play a role?
McCarthy: It is an important consideration. Patients who are diabetic or morbidly obese have a slightly higher incidence of infection than patients without those conditions. That is not to say that you cannot do a hip replacement in somebody with diabetes, hypertension, cardiac disease, pulmonary disease, or obesity, but the physician and patient must collaborate before the surgery to make the best preparation to optimize the outcome.
Is it important to undergo a dental evaluation prior to surgery in case periodontal infection is in the bloodstream? Are there other precautionary measures people should take?
McCarthy: Yes, a dental evaluation is important. Surgery of any kind is a stress to the system. Many patients are less than cognizant of how the procedure will affect them, particularly if they’re undergoing the procedure in their 60s or 70s. We would discuss heart or cardiac issues and advise a visit to a cardiologist, particularly if a patient has high blood pressure, irregular heartbeat, a family history of heart disease, or other potentially complicating conditions. At times, we discover that a patient does have cardiac abnormalities and needs treatment before surgery to lessen risk.
In addition to the dental and medical evaluation, particularly of the cardiopulmonary system, many women suffer from underlying asymptomatic urinary tract infections that should be identified and treated before surgery.
Also, many patients may be unaware of venous insufficiency or swelling of the calf and leg. Many of these patients have mild high blood pressure, and their legs swell towards the end of the day because their veins are not working at optimal capacity. Some of those patients are at higher risk for developing blood clots, so we screen people ahead of time. If there’s any history of a blood clot or abnormal findings, we’ll perform an ultrasound test to make sure they don’t have a blood clot in the leg already and put them on a low dose of a blood thinner before the surgery as a preventive measure.
How soon after hip replacement can a person resume their normal routine?
McCarthy: Generally speaking, younger, healthier patients go home in a couple of days, while others with medical issues may leave in three or four days.
Many years ago, people were kept on bed rest for days and weren’t allowed to do anything for six weeks or more. Now, we stand patients up the night of surgery. They’re walking the day after surgery, climbing stairs the following day, and often driving within the first two weeks–it used to be months. After their wound has healed in a week or two, patients can get in the pool and exercise. Many patients, even in the first week or two, can do gentle stationary biking. In terms of functional activities such as golf, it used to be from three to six months before patients could return to the links, but now they are returning to the sport in less than half that time.
What can individuals do after their surgery to preserve the integrity of the procedure and make it last longer?
McCarthy: There needs to be an initial healing, or knitting, of the implant to bone. If the implant is a noncemented bony in-growth implant, that biology occurs over three to six months. Although they can use it immediately and it’s very rigidly fixed, there is still healing. Even though you fix an ankle fracture, for example, it takes three to six months for the bone to fully repair itself. A similar time frame is true when knitting the prosthesis to the bone. Use comfort as your guide. Don’t overdo it.
Second, patients want to avoid complications like blood clots, infection, and dislocation. We remind them in the office about the importance of dental prophylaxis and avoiding infection.
Third, it is important to develop not just a sense of comfort in the joint, but to improve the flexibility and strength of the muscles around the joint, because the muscles act like shock absorbers, just like in your car–the better your shock absorbers, the less the wear and tear on the car itself.
We encourage regular exercise to help regain flexibility as well as to develop power, strength, and endurance—walking, swimming, stationary biking, or cross country skiing. We discourage high-impact or “bouncing”-type sports, such as running five miles a day, playing full-court basketball four hours a day, bungee jumping–any activity that exerts a great impact on the joint repeatedly.
How can one help prevent the need for hip replacement?
McCarthy: There’s a tremendous amount of research under way on prevention by researchers through funding from the National Institute of Musculoskeletal Health at the NIH. In the last 30 years, one profound problem that we face in the United States is the dramatic increase in obesity, a huge, confounding variable when it comes to preventing arthritis. If one is obese, the forces on the joint are far worse. Another factor is that with advances in medical treatment, people are living longer, so the prevalence of arthritis is going up. In terms of research, a great focus of research is at the molecular and genetic level, looking for mutations that may predispose someone, or families, to arthritis.
The National Center for Complementary & Alternative Medicine at the NIH is conducting research on the potential of the over-the-counter supplement chondroitin and glucosamine. Are the results out as yet?
McCarthy: The trial results are not yet in. We don’t discourage people from taking the supplements because there are very few side effects so far. There are isolated reports that have demonstrated some benefits, but corroboration is what makes medical science. That really has not occurred, so school is still out on that issue.
Become a Saturday Evening Post member and enjoy unlimited access. Subscribe now



Comments
I am an active 89 year-old who has a date in April for a hip replacement. For the past 10 years I’ve been doing half and whole marathons. I started runnning late in life because I have quite a bit of scarring in my leg and my circulation was starting to be compromised. My ortho surgeon is not young so I’m concerned that he’s not up on the latest although he performs many replacements. Since my insurance is an HMO, I don’t have a lot of options as to hospitals, surgeons, etc. I’d like some reassurance that it’s safe for me to proceed with the surgery at my age and with the scarring. Anyone have some advice?
My son is 18 years old and was diagnosed with Femoral Acetabular Impingment at the age of 17. He had bilateral hip surgery to repair the labrum tears and reshape the femoral head. He faired well in the first surgery and his surgeon was able to repair everything. The second surgery, which was done on his left hip, did not go as well. There were labral tears, which were repaired, but there was also articular cartilage damage in the acetabelum which could not be repaired. We were told that my son has developed osteoarthritis in his hip and that there is no way to repair it due to the fact that there hasn’t been a way for surgeons to “glue down” the articular cartilage. I am reading everything I can get my hands on to find out if there is something that can be done. Does stem cell engineering or osteochondral allograft transplantation work in these cases? My son’s surgeon has informed us he will need a hip relpacement in his young adult life, most likely, depending on the circumstances of his activity level, in his late twenties or early thirties. My son is so much pain right now, I can’t imagine him dealing with this for another 10 years or longer. Do you have any suggestions for me? Do you recommend a particular hip surgeon or facility? I really appreciate any help you can give me. Thank you.
Any back exercise routine worth its salt includes work for the oblique abdominals. The oblique abdominals consist of 2 pairs of ab muscles. There’s an internal oblique and an external oblique on each side of the trunk (in front). The obliques enable you to twist and tilt your spine, and they help stabilize the trunk, otherwise known as the core.
This beginner level exercise involves an ab crunch (or ab curl, if you’re into Pilates) combined with a rotational movement of the shoulder. Experts recommend doing a back exercise routine every day — this exercise can be included in your routine on some or all days.
I am going to give the ok to go ahead with hip replacement. I can not do much without being in pain. I just hope recovery is quick. Jobs are hard to hang on to these days. I also hope to be able to go horsebackriding again.
I just got the news in the mail today, and I was extremely troubled by the x-ray that I had the first of the week. I now need a MRI to clearly see what type of damage there is.. The plain x-ray showed a subchrondal fracture identified at the femoral head, with large depressed triangular, dome shaped fragment that was 4.3 cm in diameter. I really do not know what all this is about, as I have been in shock since I opened the letter from my doctor requesting a stat MRI. I have read this letter and put my mind somewhat at ease. (If that is possible with me) I tend to be on the anxiety highway, and this is no exception. I fell about 6 weeks ago, doing something that I am finding out that I am too old to engage in. Roller skating; I thought that would be dandy exercise for both myself and my dog, which loves to run. I found both feet to be in the ‘splits’ position, so I crawled to the grass to get up. It was then when I said, ‘one fall, that’s all and sold my skates. I just turned 55 and very young at heart, however my body is telling me different. Anyone out there that has had this problem and can give me some comforting help.
My 52 year old son has had an infection in his blood for 3 years and ha been hospitalized many times. Dr(s) have been unable to eliminate infection which they say is destroying bone in hip. He is in constant pain and walks using a cane when he feels well enough to be out of bed. Dr now wants to remove total hip joint. Dr says he will be able to walk only with a walker- not with cane. Dr vague about eventually replacing hip (ball & socket) with prothesis.”Maybe in 4-5 years if infection all gone”
Any recommendations???
The article is EXCELLENT!!, it answered a lot of my questions about hip implants, recovery time after surgery and things I can do to streghten my hip muscles such as pilates, pool therapy etc.
I live in La Paz, Bolivia and I would really appreciate it if you could please send me the address of some hospitals and physicians in the States who specialize themselves in hip implants, since I am planing to have my surgery in the US.
Thank you very much,
Cecilia Rojas
I am 58 years young…alway exercised, and have been dealing with OA for years. It has progressed to the point where now, I have bone on bone and worse in both knees and both hips.! I am limping so bad..I can barely walk..I have done everything possible to postpone surgery…cortisone, glucosamine, swimming, lost 40 lbs., those chicken comb shots in my kneest really have fought this thing.. I can’t pick up my grqndchild any more and I am her care giver…..so I will have a hip replacement in my left hip next month. Then I need to do the rest of me. I want to have aan active life again…so I hope to do all my joints within a year or so. What is the righ tamount of time to wait between surgeries.?
I just found out today from my doctor that I need a right hip replacement and I am 49 years old. Being that I have Rhuematoid Arthritis I am in a lot of pain daily and will be glad that after my hip replacement I should not have as much pain in my hip. The only thing is that I was also told that my condition could happen in other joints due to my medicine that I am on for my RA. I am contemplating going off of the medicine that is keeping my RA pain down so that it will not kill my joints. You see the joint that I am having to replace does not have any blood in it and it is due to the Prednisone that I am taking for my RA. If anyone has any ideas for me to keep the pain of RA down without the help of Prednisone please let me know. Thank you 🙂
I had a total hip replacement on my right side on july 7 2009.I was walking(with a walker) on the third day. Perhaps I can attribute this rapid advance to the fact that I wanted to get the hell out and smoke a cigarette!
I am 51 years old and as much as I would like to give the credit to the doctor,I have to say it was my attitude that caused such a rapid assent towards the healing prosses.
The only caveat I have to offer is this: Whoever the doc is,go to a hospital where they will treat you well!
I was treated like crap.
Dom
the information in the article is excellent. i have had total hip replacement on one hip and need to have the second one done now,
4 1/2 years later. i am a physically active 70 year old, and will probably opt for the least invasive procedure.
i note that the interview date in Nov 01, 05 – almost 4 years ago. it certainly would improve my knowledge and update my research to have a similar, current article of this type.
thanx, PKerr