Your Health Checkup: Marijuana and Your Health
“Your Health Checkup” is our online column by Dr. Douglas Zipes, an internationally acclaimed cardiologist, professor, author, inventor, and authority on pacing and electrophysiology. Dr. Zipes is also a contributor to The Saturday Evening Post print magazine. Subscribe to receive thoughtful articles, new fiction, health and wellness advice, and gems from our archive.
Order Dr. Zipes’ new book, Bear’s Promise, and check out his website www.dougzipes.us.
When I wrote about marijuana (cannabis) previously, I emphasized that its legalization in multiple states as well as increased recreational use, especially among young people, have heightened the need to better understand its potential benefits and harm. Because multiple formulations exist, including edibles, transdermal formulations, combustible smoking, and vaping, assessment is difficult since each can impact health differently.
In general, marijuana exposure impairs thinking, psychomotor skills, and driving ability, and can inflame bronchial airways, leading to bronchitis. While the adverse cardiovascular effects are less certain, multiple reports have noted heart rhythm problems such as atrial fibrillation, ventricular tachycardia (rapid heart rates from the bottom heart chamber), and acute coronary syndromes such as heart attacks, cardiac arrests, and strokes.
The most definitive report on medical and recreational use and cardiovascular health has just been published as a scientific statement from the American Heart Association. They note its beneficial effects on pain, cachexia (wasting), nausea, vomiting and spasticity, but that there are no well documented beneficial effects on the heart and blood vessels.
Multiple compounds, particularly tetrahydrocannabinol (THC) and cannabidiol (CBD), determine the impact of cannabis products that can contain pure THC or CBD or their combination. The two compounds exert profoundly different actions on the heart and blood vessels. THC exerts generally negative actions by stimulating the system of nerves (sympathetic nervous system) that increases heart rate, need for oxygen by the heart muscle, blood pressure, and platelet stickiness, and makes the inner lining of blood vessels function abnormally. The increase in oxygen demand by the heart and decreases in heart muscle oxygen supply can trigger angina or even heart attacks in people with preexisting coronary artery disease, particularly when cannabis is smoked.
CBD appears more beneficial than THC and may reduce heart rate and blood pressure, improve blood vessel function, and reduce inflammation. CBD is non-psychoactive, is found in cannabis plants like marijuana and hemp, and has no recreational application. The only investigations of CBD subjected to rigorous study are those for epilepsy and schizophrenia, so claims of benefits for a host of other illnesses remain unsubstantiated.
Cannabis can have addictive qualities with long term exposure, and users may experience withdrawal symptoms such as anger, anxiety, restlessness, irritability, depressed mood, disturbed sleep, strange dreams, decreased appetite, weight loss, headache, and night sweats if cannabis is suddenly stopped, the dose is reduced, or formulation changed. In addition, tolerance occurs with chronic use.
Except for nicotine, adolescents abuse cannabis more than any other drug. Because the brain continues developing until approximately 21 years, adolescent exposure to marijuana can be particularly harmful. Use before age 16 or 18 has been associated with poorer sustained attention and reduced verbal IQ, along with abnormal structural changes in the brain. Pregnant women or those considering becoming pregnant should refrain from using cannabis because of potential damaging effects on the fetus.
Before using cannabis, consider potential risks and benefits for the various forms of drug and administration. Cannabis obtained from the black market, especially synthetic illicit cannabinoids, should be avoided because of possible adulteration, contamination, and questionable dosages. Smoked or vaporized cannabis in general should be shunned, especially in patients with respiratory diseases. Cannabis should not be used in combination with alcohol or drugs that affect mental activity. People with psychiatric conditions should avoid compounds containing primarily THC with little or no CBD.
Many rumors and fallacious claims about the health benefits of cannabis products exist, and users should be wary. If something sounds too good to be true, it usually is.
Featured image: Cannabis plants (Tatevosian Yana / Shutterstock)
Your Health Checkup: Breakfast, Diet, and Exercise
“Your Health Checkup” is our online column by Dr. Douglas Zipes, an internationally acclaimed cardiologist, professor, author, inventor, and authority on pacing and electrophysiology. Dr. Zipes is also a contributor to The Saturday Evening Post print magazine. Subscribe to receive thoughtful articles, new fiction, health and wellness advice, and gems from our archive.
Order Dr. Zipes’ new book, Damn the Naysayers: A Doctor’s Memoir.
In my last column, I discussed the risks of eating eggs for breakfast. I hope that information encouraged readers to substitute another food, such as bananas, yogurt, or cereal and fruit, and not stop eating breakfast, since skipping breakfast entirely appears to carry its own risk.
Investigators analyzed the eating habits of a nationally representative group of 6,550 participants aged 40 to 75 years (with a mean age of 53 years, almost half males), and followed them for 17 to 23 years. After adjusting for multiple confounding factors (always a weak point in such studies), they found that participants who never ate breakfast compared with those who ate breakfast everyday had an 87 percent increased risk for cardiovascular mortality and a 19 percent increased risk for death from any cause.
The authors noted that breakfast is an important meal, but almost 25 percent of young people skip it every day. They cite a host of health risks from doing so, including obesity, lipid problems, hypertension, diabetes, and coronary and cerebrovascular disease. This study doesn’t prove causality but only an association and other factors may be important as well.
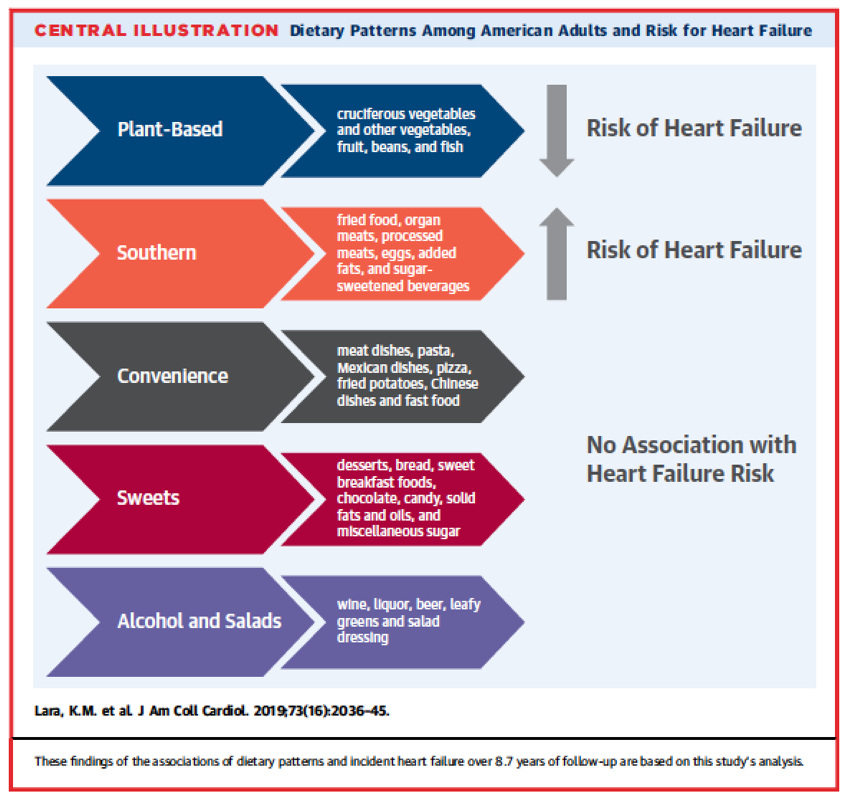
As I have stressed, what you eat is as important as when you eat. In a study of 16,068 individuals with a mean age of 64 (slightly more than half women and a third African American), the authors evaluated five types of diet: plant-based, southern, convenience, sweets, and alcohol and salads (see figure.) Those individuals adhering to a plant-based food diet including vegetables, beans, fruit, and fish enjoyed a 41 percent reduction in heart failure. Those who ate a diet loaded most heavily with fried foods, organ meats, processed meats, eggs, added fats, and sugar-sweetened beverages had a 72 percent increased risk of heart failure. The results of this study show that adhering to a plant-based diet reduced heart failure risk in a diverse population of American adults, even when they had hypertension, a known risk factor for heart failure.
Another recent study of over 400,000 men and women from nine European countries followed for 12 years found essentially the same dietary risks for red and processed meats, in this instance causing coronary artery disease (heart attacks).
And finally — I know I keep harping on it— physical activity is critically important. People can offset the impact of sitting at work all day, which is associated with an increased risk of all-cause and cardiovascular death among the least physically active adults, if they perform moderate-to-vigorous physical activity in doses that meet current recommendations.
Because walking and vigorous physical activity can most consistently reduce the risks of cardiovascular disease and premature mortality caused by sitting all day long, go do it, starting today! Walk the dog, play ball with your kids, join a fitness center, but do something!
Featured image: Shutterstock.com
Your Weekly Checkup: Childhood Violence and Workplace Bullying May Be Bad for Your Heart
“Your Weekly Checkup” is our online column by Dr. Douglas Zipes, an internationally acclaimed cardiologist, professor, author, inventor, and authority on pacing and electrophysiology. Dr. Zipes is also a contributor to The Saturday Evening Post print magazine. Subscribe to receive thoughtful articles, new fiction, health and wellness advice, and gems from our archive.
Order Dr. Zipes’ new book, Damn the Naysayers: A Doctor’s Memoir.
In September 2018, I wrote about the adverse physical effects of psychological stress and made the point that psychological stress had a strong, dose-dependent association with heart attacks and strokes in men and women, possibly via an increased inflammatory state. Recent information has expanded that association to include violence in youngsters and workplace bullying.
Violence can take many forms, including racism, incarceration, economic deprivation, policing, individual decision making, and access to guns. Even spanking children as a disciplinary measure can be a form of violence. These factors create a post-traumatic stress disorder among exposed individuals.
Childhood exposure to community violence may manifest in cardiovascular disease later in life. Studies in Mississippi and Sweden have found an increase in cardiovascular disease in both men and women from neighborhoods where community violent crime or unemployment increase. Violence stresses the brain and modulates nerves that control heart and brain function. The body adapts to various stressors over time in ways that can be harmful, and result in abnormal metabolic changes, diabetes, or coronary artery disease.
Depending on the level of violence, brain structure and function can change. Adults who reported violence in childhood have also been found to have increased inflammation. By the time children reach adulthood, violence is statistically linked with cardiovascular disease, with a threefold greater risk of cardiovascular disease for every seven adverse childhood events.
While difficult work conditions, including job strain and excessive hours, have long been linked to an increased risk of cardiovascular disease, the impact of bullying on heart disease has only been studied recently. Bullies were colleagues, supervisors or subordinates, rather than clients or other individuals outside the workplace.
People who are bullied or exposed to violence on the job appear to be more likely to develop cardiovascular disease than individuals not exposed to these challenges at work.
Researchers examined survey data from more than 79,000 employed men and women 19 to 65 years old without a history of heart disease. About 9 percent reported being bullied and 13 percent said they had been exposed to violence on the job in the last year.
Those bullied on the job were 59 percent more likely to be diagnosed with heart disease or hospitalized for heart attacks or strokes in subsequent years than those who were not bullied, while workers exposed to violence had a 25 percent higher likelihood of developing heart disease or hospitalization for related events. The associations showed a dose–response pattern for workplace bullying and to a lesser extent also for workplace violence. The authors concluded that bullying and violence are common at work, and those exposed to these stresses are at greater risk of developing cardiovascular disease in the future.
Violence in youngsters and bullying in the workplace likely do not occur in isolation but are part of a continuum of risk behavior beginning at a young age and continuing into adulthood. If the associations demonstrated are actually causal, that is, violence and bullying directly cause cardiovascular disease, then interventions to resolve interpersonal problems beginning with children and continuing as lifelong endeavors would be expected to prevent a sizable number of cardiovascular events from occurring in the future.
Your Weekly Checkup: Electronic Cigarettes Revisited
“Your Weekly Checkup” is our online column by Dr. Douglas Zipes, an internationally acclaimed cardiologist, professor, author, inventor, and authority on pacing and electrophysiology. Dr. Zipes is also a contributor to The Saturday Evening Post print magazine. Subscribe to receive thoughtful articles, new fiction, health and wellness advice, and gems from our archive.
Order Dr. Zipes’ new book, Damn the Naysayers: A Doctor’s Memoir.
I have written previously about vaping and the use of electronic cigarettes. I stated that an expert committee of the National Academies of Sciences, Engineering, and Medicine concluded, “There is no available evidence whether or not e-cigarette use is associated with clinical cardiovascular outcomes (coronary heart disease, stroke, and peripheral artery disease) and subclinical atherosclerosis (carotid intima media-thickness and coronary artery calcification) but that heart rate…and blood pressure rose acutely after e-cig exposure.” I wrote in April that vaping may be safer than traditional smoking, but we needed more studies to be sure. I also noted that nicotine is addicting, whether in an e-cigarette or conventional cigarette.
More recent information requires an update of those comments.
Many people smoke e-cigarettes for one of three reasons:
- They think e-cigarettes are safer
- They believe they can smoke them in places where they are not allowed to smoke conventional cigarettes
- They use them to quit smoking conventional cigarettes
All three of those beliefs appear to be wrong. E-cigarettes do not appear to be safer, they are often forbidden in the same places conventional cigarettes are forbidden, and they actually may make it harder to quit conventional smoking.
Researchers at the University of California, San Francisco, analyzed data from 69,725 people who underwent in-person interviews as part of the National Health Interview Surveys in 2014 and 2016. Respondents characterized their use of traditional or e-cigarettes by choosing never, former, some days, or daily. Researchers found that most adults who used e-cigarettes continued to smoke traditional cigarettes.
Daily e-cigarette use appeared to be independently associated with an elevated risk for heart attack, as was daily conventional cigarette use. Transitioning completely from cigarettes to e-cigarettes was still associated with an increased heart attack risk since e-cigarettes pose an independent risk different than cigarettes. Some of the mechanisms by which they act are common, but there are independent effects. E-cigarettes represent a different kind of toxic exposure.
Daily use of electronic cigarettes almost doubled a person’s risk for heart attack, while those who reported daily use of both electronic and conventional cigarettes appeared 4.6 times as likely to have a heart attack than those who never used either product.
A primary toxic agent in e-cigarettes may be the ultrafine particles contained in the aerosol created by heating a liquid solution of nicotine. Those ultrafine particles have serious negative short-term and long-term effects on cardiovascular function. In addition, the nicotine impacts the nervous system in ways that are associated with heart disease risk. There are many strong oxidizing chemicals in e-cigarettes — such as acrolein — that are associated with heart disease risk. Harmful effects can occur within minutes.
For those with lung cancer, e-cigarettes appear to deliver a lower level of cancer-causing chemicals than traditional cigarettes, but the cardiovascular effects are very serious. Exposure to nicotine can make cancer worse by promoting growth of blood vessels into tumors, as well as other changes that may make tumors grow faster. I would not recommend e-cigarettes for conventional smokers with lung cancer.
Many strategies exist to help people stop smoking, such as nicotine replacement therapy or prescription drugs, combined with counseling, and work quite well for motivated individuals. If individuals are already using e-cigarettes and do not want to change, at the very least they should stop combined use with cigarettes.
I’ll reiterate the advice I gave in April: The safest recourse is not to smoke. Period!
Pass the Fish Tacos, Please

There’s solid proof that omega-3s support cardiovascular, cognitive, and joint health. But an important question lingers in the air: Do seafood and fish oil supplements offer equal protection?
“Fish oil supplement is not the same as eating whole fish. In fact, recent research found that omega-3s in capsule form may not provide any actual benefits to your heart health. That’s why I recommend my patients follow the Dietary Guidelines for Americans and consume 2 to 3 servings (8 to 12 ounces) of seafood each week,” says Dr. Lori Mosca, Professor of Medicine at Columbia University Medical Center and Director of Preventive Cardiology at New York-Presbyterian Hospital.
Interestingly, both women and men need the same amount of fish each week to support heart health and reduce heart disease risk. One serving is about the size of the palm of your hand, says Dr. Mosca who offers these simple ideas for powering family meals with omega-3s by replacing your usual protein with fish:
Breakfast option: Top a multigrain bagel with canned tuna.
Lunch option: Fill tacos with fish, or add fish to a green salad.
Dinner option: Grill salmon, or stir fish into a pasta sauce.
For more recipes visit GetRealAboutSeafood.com.