The New Science of Stress
The irony is not lost on Barbara Joyce, a teacher from Tenafly, New Jersey. The 52-year-old wife and mother of three has plenty of stress in her life, from the beating her retirement savings took during the 2008-2009 financial crisis to her two daughters’ struggles to find employment in the jobless recovery. And to top it off, she was in Tokyo during the March 2011 earthquake and tsunami. Since her doctor reminded her that stress can hurt her health, she has taken up jogging, and says she “literally runs off stress.” She can’t escape it entirely, though, and worrying that it is increasing her risk of cardiovascular disease, arthritis, and possibly some forms of cancer causes her … even more stress.
The suspicion that there is a connection between psychological stress and health—especially heart health—goes back to antiquity. In the mid-20th century endocrinologist Hans Selye coined the term “stress,” and described how the chronic, unrelieved kind can cause pathology, largely through the release of stress hormones including cortisol and adrenaline. Now advances in molecular biology and neuroscience have brought good news and bad news about stress and health. The bad news is that newly discovered mechanisms triggered by an overload of stress cause changes in neurons and the immune system that are more extensive than ever before suspected—with consequences for conditions as varied as asthma, arthritis, hypertension, and HIV/AIDS. The good news is that there are more ways than ever to reduce stress, even if you don’t feel like strapping on a pair of running shoes.
Anecdotal evidence of how stress impairs health is everywhere. Ed Rogers, 66, a public health consultant in Louisville, Kentucky, swears that whenever his wife yells at him for shirking his share of the housework he has to grab his inhaler to stave off an asthma attack. Whenever David, 64, of Breckenridge, Colorado, gets “tired and frustrated by the turkeys one is forced to work with/for,” he says, it causes “tension in the shoulders and neck tending toward headaches.” (Not wanting to offend those “turkeys,” David asks that his last name be withheld.)
But the evidence goes beyond anecdote. Chronic stressors such as financial, work, or marital problems plus the attendant depression, hostility, and anxiety account for about 30 percent of heart attack risk calculate a team of Swedish scientists. And high levels of the stress hormone cortisol strongly predict the likelihood that someone 65 or older will die of cardiovascular disease, as scientist Nicole Vogelzangs of VU University Medical Center and colleagues in The Netherlands found in a 2010 study. Previous research had “suggested that cortisol might increase the risk of cardiovascular mortality, but until now, no study had directly tested this,” said Vogelzangs. But her work found that people in the top one-third of cortisol levels are five times more likely to die of cardiovascular disease than those in the bottom one-third.
In one of the most elegant demonstrations of the link between stress and heart attacks, researchers at The University of Western Ontario (UWO) measured cortisol levels in hair, which is like examining tree rings to determine when droughts and other climate calamities occurred. Hair grows about 1 centimeter—just under half an inch—per month, explains UWO’s Gideon Koren, “so if we take a hair sample six centimeters long, we can determine stress levels for six months by measuring the cortisol level.” Using that approach on 56 men who had recently suffered a heart attack, he and colleagues found that the men had higher cortisol levels in the previous three months than comparable men hospitalized for other conditions, they reported last year.
“Experiments of nature” have offered dramatic demonstrations of the deadly effects of stress. Immediately after the 1994 Los Angeles earthquake, the number of cardiac deaths spiked two to five times the normal rate. And after the 9/11 attacks, the rate of defibrillator firings over the next month was two to three times normal, as the number of people whose heart needed to be shocked back into a normal rhythm soared as a result of chronic stress. But stress that falls short of the Richter scale and a terrorist attack can also harm health. Work, not surprisingly, is the stress mother lode. People working 50 hours a week or more are 13 percent more likely to report hypertension than people working 40 hours a week, and a stressful job with little decision-making authority raises blood pressure rates even during sleep.
Stress can harm health in two basic ways. One is by leading us to fall into unhealthy habits such as sleeping poorly, being less likely to exercise, smoking, and eating unhealthy foods (especially sugars and fats). The American Heart Association reports that 20 percent of Americans are worried that stress will affect their health—yet 36 percent of them say they deal with stress by drinking alcohol or eating. Result: a self-fulfilling prophecy. The poor health habits that result from stress account for an estimated two-thirds of the additional risk of heart attack and other cardiovascular illnesses in people with depression and anxiety, found a 2008 study in the Journal of the American College of Cardiology.
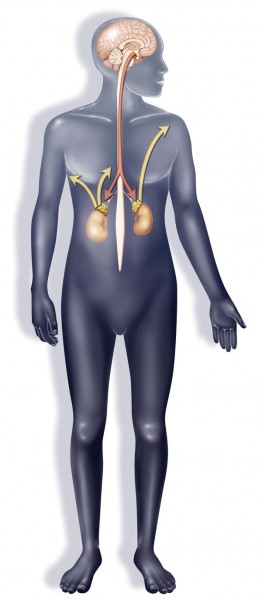
The other path from stress to illness winds through the endocrine, or hormone, system. Stress causes the brain’s hypothalamus to send a message to the adrenal glands, which sit just above the kidneys, to release cortisol. That may seem like a design flaw, but in fact cortisol helps the body recover from acute stress, including by raising blood sugar—the better to help you flee a saber-tooth cat. (The adrenals also release adrenaline, or epinephrine, and the related norepinephrine.) But trouble begins when too much cortisol is released, or when it is released unnecessarily—that is, not in response to an actual and immediate threat but to background anxiety—and remains chronically elevated. High cortisol levels cause chronic inflammation, which can cause arthritis to develop or worsen, and trigger the release of immune-system proteins called cytokines, implicated in such age-related diseases as Alzheimer’s, Parkinson’s, and type 2 diabetes.
How Stress Impairs Health
In Greek mythology, the monstrous Hydra terrorized visitors to a mystical lake. Beheading the Hydra was no easy task because it grew two new heads whenever one was cut off. The multiplying evil of the Hydra offers an apt analogy to the insidious ill-effects of stress in modern life. Chronic high levels of stress bring on a world of trouble on multiple body systems and can lead to…
Worsening of Asthma symptoms
This condition is marked by inflammation of the airways, so it’s no surprise that stress, by causing inflammation, increases asthma symptoms. A University of Wisconsin study showed how. When students with asthma inhaled an allergen (ragweed, dust mites, or cat dander), lung inflammation was 27 percent higher during finals than during a low-stress period—even though the allergen exposures were identical.
Cardiovascular disease
Stress increases blood levels of inflammatory molecules (called IL-6, C-reactive protein, and fibrinogen). These bad actors promote the development of atherosclerosis, or hardening of the arteries. The inflammatory molecules that trigger atherosclerosis also make the fatty arterial deposits called plaques more likely to rupture, causing a heart attack or stroke. Stress also causes the nerves to flood the bloodstream with a molecule called neuropeptide Y (NPY), which raises heart rate and blood pressure. NPY stimulates the growth of abnormal smooth muscle in blood vessels, which leads them to become blocked with plaque-like deposits of microphages, thrombus, and lipids.
Faster weight gain
NPY also seems to be the culprit behind our tendency to overeat and gain weight when we’re stressed. It throws a monkey wrench into the brain’s appetite-regulation system, and can also “unlock” receptors in fat cells, stimulating them to grow in size and proliferate. That also seems to be an evolutionary adaptation—early humans benefited from putting on fat in response to stress, which tended to be of the “mammoths are scarce this year” variety rather than the “I can’t make my mortgage payment” kind. As a result, a physiological response that was adaptive in the past is harmful today: We put on a nice layer of fat that doesn’t actually help us cope with the source of our stress. The effect is so powerful that stressed mice on high calorie diets gained twice as much fat as unstressed mice on the same diet.
High cholesterol
One reason mental stress can raise cholesterol levels may be that stress encourages the body to produce more energy—to fight or flee—including fatty acids and glucose. Both substances cause the liver to produce and secrete more LDL, or bad cholesterol.
Impaired immune system
Although scientists have long suspected that stress undercuts the immune response, only now has the mechanism behind that connection become clear. When we are stressed, the flood of NPY impairs the immune-system cells whose job is to fight infections. As a result, colds, flu, and other viral diseases are more likely. So are virally caused malignancies such as cervical cancer, which can be triggered by the human papillomavirus (HPV). HPV infection alone is not sufficient; the immune response causes most HPV infections to disappear. But, with stress in the mix, precancerous cervical lesions are more likely to progress to cancer.
Weakened response to HIV
Stress can bring about changes that allow the HIV virus to replicate more quickly, accounting for much of the variability in how people respond to an HIV infection. By keeping stress under control or avoiding stressors an HIV-positive person is more likely to remain asymptomatic for long periods rather than progressing to AIDS and is less likely to suffer opportunistic infections.
Increased risk of dementia
Psychological stress in middle age can raise the risk of dementia, especially Alzheimer’s disease, in old age. Scientists at Sweden’s University of Gothenburg followed 1,400 women for 35 years, asking them about their levels of psychological stress in 1968, 1974, 1980, 1992, and 2000 to see who developed dementia. Women who reported repeated periods of stress in middle age were 65 percent more likely to eventually develop dementia than women who did not. In women who reported stress at all time points, the risk was more than twice that of women who had escaped stress. So what’s the connection? A solid body of research shows that stress hormones called glucocorticoids are toxic to neurons and to the synapses that connect them, a phenomenon dubbed “neurostress.” The fewer synapses in a brain, the less of a cognitive cushion it apparently has after age-related mental decline sets in.
Premature aging
Psychosocial stress can reach into our very DNA, altering the “telomeres” that sit at the ends of chromosomes like the plastic tips at the end of shoelaces. Telomeres become shorter as the cell (and the person) ages. When enough telomeres reach a critically short length, the chromosome unravels like a shoelace that has lost its tip, and the cell stops dividing. This can trigger or contribute to age-related diseases. People under chronic stress have shorter telomeres and less of the enzyme telomerase, which repairs that damage, find scientists led by Ronald Glaser of Ohio State University.
Increased risk of cancer
This one’s a big “maybe.” The problem for scientists is that it is almost impossible to know whether a stress-free immune system keeps nascent tumors in check. Micro-scopic tumors are almost impossible to detect, so researchers can’t tell whose are being quashed by a healthy immune system and whose are being allowed to proliferate by a stress-impaired immune system. A 2007 study found that, in cell cultures, the stress hormone norepinephrine can ratchet up biochemical signals that stimulate tumor cells to proliferate. And in multiple myeloma cells growing in lab dishes, norepinephrine can increase production of proteins that foster metastasis. “For years it was thought that the immune system plays no role in cancer,” says immunologist Peter Lee of Stanford. That’s because cancer is part of the “self,” and the immune system targets only “non-self”—viruses, bacteria, organ transplants. But now, he explains, “We and other labs have uncovered multiple immune deficits in cancer patients.”
Harm to the next generation
Stress can jump the generation gap. A mother’s stress during pregnancy can influence the baby’s developing immune system in such a way as to make the child’s immune response go into overdrive. For example, such children are at higher risk for asthma and for allergies to dust.
Learn to be Stress Free!
As science keeps uncovering more ways that stress can impair health, there is also increasing confidence that you really can learn to lower stress levels. Researchers today understand more precisely than ever what it takes to control stress.
Aerobic exercise is an excellent place to start. Regular exercise, especially when combined with stress management training, can actually decrease cardiovascular risk in patients with heart disease.
The next step is to adopt principles of what’s known as cognitive behavorial therapy (CBT) focusing on stress management. CBT includes monitoring yourself for signs of stress and learning such stress-management skills as deep breathing and spiritual development. In studies, people receiving CBT had a 41 percent lower rate of both fatal and non-fatal heart events, 45 percent fewer recurrent heart attacks, and a 28 percent lower rate of death over the eight years that they were followed.
Stress management can improve physiological markers of cardiovascular health, found a 2011 study. It was the first randomized trial to show that something other than drugs can improve blood flow to heart, health of blood vessels, and ability of the cardiovascular system to regulate surges in blood pressure.
Even the way you fight can make a difference. A 2009 study found that when couples used words to indicate that they are thinking about their conflict in a rational way rather than making accusations they experienced smaller increases in cytokines after the fight compared to couples who fought irrationally.
Proper stress manage-ment can even impact your DNA. Herbert Benson, M.D., who coined the term “relaxation response,” finds that yoga, prayer, and a meditation-like exercise he developed—sitting quietly, relaxing your muscles, breathing rhythmically, and repeating a “focus” word when you exhale for 20 minutes—all lower heart rate, blood pressure, and inflammation. And, as he describes in his book The Relaxation Revolution, these calming activities affect DNA. Comparing experienced meditators to novices, he and colleagues found that 2,209 genes were expressed differently—that is, switched on or off—in the two groups. Among them: genes involved in the immune system, inflammation, premature aging, and oxidative decay implicated in heart disease and cancer. But after just eight weeks of stress-management training, Benson finds, hundreds of genes in novice meditators moved away from the stressed-out pattern and instead resembled one that has been “associated through past research with clear health benefits.”